What you should know about COVID-19

We will update this article regularly based on the most recent medical knowledge.
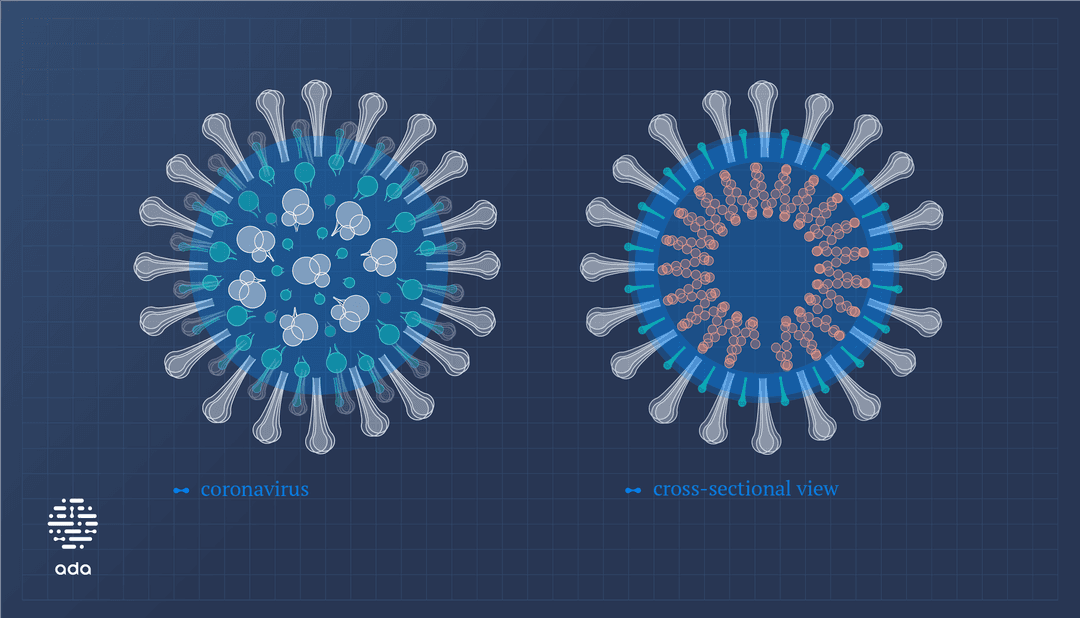
COVID-19 is a disease caused by a coronavirus called SARS-CoV-2. Scientists first discovered it in December 2019. In March 2020, the World Health Organization declared the COVID-19 outbreak a global pandemic. 1
COVID-19 usually causes respiratory symptoms, like a cold or flu, but it can also affect other parts of the body.
Most people with COVID-19 develop mild symptoms and make a full recovery. But for some, it’s a serious illness and can be deadly.
Keeping yourself informed can help you protect yourself and others during the pandemic. So let’s look at what you should know and answer some of your most frequently asked questions.
Transmission
COVID-19 mainly spreads through tiny droplets, often when an infected person sneezes or coughs but also when people talk and sing. The virus is particularly likely to spread in poorly ventilated and crowded rooms, so it’s essential you keep your distance.
You may also catch the virus by touching a contaminated surface and touching your eyes, nose or mouth. So make sure you wash your hands regularly.
Can people who aren’t sick spread the virus?
Yes. Studies suggest people who don’t have symptoms could be responsible for 40 to 45% of infections. 2
What is the incubation period?
The incubation period is the time between infection and the first symptoms. The average incubation period for COVID-19 is around 5 to 6 days but can be up to 14 days.
How long are people with COVID-19 infectious?
Current data suggest that healthy adults remain infectious for up to 10 days after developing symptoms.
Can I get COVID-19 more than once?
It’s possible but rare. 3 Infected people develop antibodies, which can protect them from another infection. But we don’t yet know how long this immunity lasts.
Risk
Are some people at more risk?
People of older age and those with pre-existing medical conditions are more likely to become seriously unwell. 4
High-risk conditions include high blood pressure, cardiovascular disease, or diabetes. 4 Children usually have milder symptoms, but there may be a link between COVID-19 and developing multisystem inflammatory syndrome. 5
Can you die from COVID-19?
Most people make a full recovery after COVID-19. However, a small percentage of people who are infected become so unwell that they die.
Symptoms
The most common symptoms of COVID-19 are: 6
- fever
- dry cough
- fatigue.
Some people also show some less typical symptoms: 6
- headache
- muscle aches and pains
- sore throat
- diarrhea
- reduced or lost sense of smell and taste
- runny nose
- red or irritated eyes.
What about long COVID-19?
Some people have symptoms that last for weeks or months after they recover from COVID-19. Some of the symptoms people report are: 7
- fatigue
- problems with concentration and memory
- headaches
- pins and needles
- loss of sense of smell
- persistent cough and shortness of breath
- digestion problems.
People are not infectious while experiencing symptoms of long covid.
What should I do if I think I’m infected?
- Stay home and rest.
- Before you go to a doctor’s office or the emergency room, call ahead and tell them you think you have COVID-19.
- Avoid contact with others, and don’t travel.
- Cover your mouth and nose with a tissue or your sleeve, not your hands, when you cough or sneeze.
- Wash your hands often with soap and water for at least 20 seconds. Use an alcohol-based hand sanitizer if soap and water are not available.
- Wear a face mask when you’re around others.
Check with your local public health authority in case there’s specific advice for your area.
Concerned? You can check for COVID-19 symptoms for free by downloading Ada now. Keep in mind that you’ll need further testing for a diagnosis.
Diagnosis
A healthcare professional can take a swab from your upper respiratory tract. That means from the back of your throat through your nose or mouth. The swab is then analyzed for coronavirus proteins at the testing site (rapid antigen test) or in a lab to detect genes from the virus (PCR test).
There are also antibody tests that may identify previous infection and possible immunity.
Treatment
There is currently no drug to treat COVID-19. In most cases, you can treat mild symptoms at home. However, when people become seriously unwell, they might need to be looked after in an intensive care unit.
Prevention
Avoiding exposure to the virus is the best way to prevent infection. Here are the standard measures to prevent the spread of COVID-19:
- Wash your hands frequently with soap and water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitizer.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Try to keep 2 meters distance from people who aren’t part of your household.
- Stay home if you have symptoms, even mild ones.
- Cover your cough or sneeze with a tissue, and then throw the tissue in the bin.
- Disinfect frequently-touched objects and surfaces.

Should I wear a mask?
Both the World Health Organization and the CDC recommend mask-wearing to combat the spread of COVID-19. 8 9 Some countries have asked people to wear masks in public to decrease infection. Make sure you always follow local guidance.
Vaccines
Several vaccines are now approved that can help protect against catching and spreading the virus that causes COVID-19. 10
Are the vaccines safe?
Yes. Scientists have carefully tested the vaccines to make sure they meet the international standards of safety and effectiveness.
Scientists and doctors continue to monitor the use of COVID-19 vaccines to make sure they remain safe for use.
It’s important to remember that the risks of vaccination are minimal compared to the risk COVID-19 poses to your health.
Are there any side effects?
For some people, yes. The vaccines will trigger your immune system to develop your body’s protection against the virus. When this happens, it’s normal to experience mild side effects like fever, headache, or muscle aches, although not everybody does. If you do experience side effects, they should go away quickly.
Your doctors will speak to you about side effects before your vaccination.
Think you might be experiencing side effects? You can check your symptoms for free by downloading Ada now.
Should anyone avoid the vaccine?
It’s safe for most adults to take the vaccine. But if you experience severe allergic reactions, have a weakened immune system or autoimmune disease, are pregnant or breastfeeding, or have any other concerns, discuss them with your doctor.
The COVID-19 vaccines are currently being tested in children. 10
You should still receive the vaccine if you've already had COVID-19. 10 If you were recently infected, check vaccination timing with your family doctor.
Perspective
Can I go to a doctor for non-COVID-19 complaints?
Yes. You must continue to take care of yourself through the pandemic. There is evidence that people are experiencing worse health outcomes because they are delaying seeing the doctor during the pandemic.
So make sure you go to the doctor if you need to and continue to attend any other health appointments. If you’re having any trouble with your mental health because of the pandemic and lockdown measures, your doctor can help you.
When will the pandemic be over?
It’s still hard to say as the situation continues to change rapidly.
We may have to learn to live with COVID-19 like the flu or common colds. 11
We may need booster vaccinations or to reintroduce preventative hygiene practices from time to time if infections rise again. 11

Keep reading. You can learn more about COVID-19 in our Medical Library.
World Health Organization (2020). WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Accessed on June 1, 2021.
Acp Journals (2020). Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review. Accessed on June 1, 2021.
CDC (2024). About Reinfection. Accessed on March 7, 2025.
Mayo Clinic (2024). COVID-19: Who's at higher risk of serious symptoms?. Accessed on March 7, 2025.
CDC (2024). Signs and Symptoms of MIS. Accessed on March 7, 2025.
World Health Organization (2023). Coronavirus disease (COVID-19). Accessed on March 7, 2025.
NHS (2023). Long-term effects of coronavirus (long COVID). Accessed on March 7, 2025.
World Health Organization (2023). Coronavirus disease (COVID-19): Masks. Accessed on June 1, 2021.
CDC (2023). Community Respirators and Masks. Accessed on March 7, 2025.
World Health Organization (2024). Coronavirus disease (COVID-19): Vaccines and vaccine safety. Accessed on March 7, 2025.
Jama Network (2021). The Potential Future of the COVID-19 PandemicWill SARS-CoV-2 Become a Recurrent Seasonal Infection?. Accessed on June 1, 2021.